Today I’d like to chat with you about Premenstrual Dysphoric Disorder (PMDD), which, in simplest terms, is an intensity of physical and mental symptoms caused by a change in hormones, up to two weeks prior to menstruation, to the point of significantly impacting a woman’s functioning (social, work, school, relationships). This is different from the more commonly referred to Premenstrual Syndrome (PMS) which is not a diagnosable disorder.
I’ve always had a special interest in women’s mental health and over the past decade of providing therapy for mental health and addictions, I’ve seen the impact hormones, and the menstrual cycle, can have on a woman’s mental health. Up to 12% of women experience a premenstrual disorder, which is more severe than PMS.
My interest actually began for personal reasons. In 2007-2009 my mental and emotional health were the worst they have ever been. In 2007 I was beginning my fifth consecutive year of university, had significant student debt, sold my home and moved across the country for graduate school as a therapist.
It was the fall of 2007 that I also developed panic disorder and had severe compassion fatigue.
I began to journal daily and I noticed what I call the cycle of bathroom floor days.
Every few weeks, I would find myself feeling very raw, and by that I mean I felt a higher level of sadness about things (losses in my life, things I’d hear in the news, my client’s experiences). The sadness felt so intense on a physical level. My body felt heavy, I would feel nauseous. I would be tearful quite easily. I physically hurt for the sadness I experienced and for the sadness my clients experienced. Aside from those days, depression was not something I experienced.
During these days, my generalized anxiety also peaked. I worried about all the potential bad things that could happen to me or my loved ones. Racing heart,shallow breathing, dizziness, agitated, fidgety, unable to relax and an almost debilitating feeling of dread.
It seemed that whatever I was most insecure about at the time (school,relationships, finances, health) would be magnified and my mind would tell me stories about how poorly I was doing in those areas and shame me for the choicesI made. This usually resulted in me crying, while journaling, on the bathroom floor, while running a bath.
If I was concerned about the amount of time I was spending on school/work my mind would say things like, “you should be spending more time with family, what if something bad happens and they aren’t around, you’ll feel horrible for not spending more time with them” (I actually spoke with my family on a daily basis)
If I was worried about my finances my mind would say, “you’re never going to pay off your student debt, why didn’t you work more while you were in school, you’re going to spend years trying to pay it all off, you can’t even make decent money in this field, why did you choose this field, you’ve just spent five years in school and all you have to show for it is massive debt, an ulcer and feeling terrible all the time” (I actually worked 2-3 jobs most of university and, at times, really enjoyed my work).
If I was sad about just how intense my sadness and worry was, and that it kept coming back no matter what I did, my mind would say, “What the — , you’re a therapist, how are you not managing your emotions?!? You’re such a hypocrite, you help people with this every day and can’t even manage your own emotions. Clearly you don’t know what you’re doing because you keep ending up here.” (I actually did go see a therapist).
The thing is, the good things I did and my strengths didn’t matter during these times. I focused on the negative and felt it so intensely. I imagined all the worst case scenarios and the physical sensations that came with this sadness and anxiety was debilitating. The more I journaled the more I saw this monthly pattern.
I also had physical symptoms, severe cramping (to the point of not being able to get out of the fetal position), bloating, headaches. But for me, the physical pain was nothing compared to the mental and emotional pain.
What is interesting in my journey, is that in 2007 I had to go off the birth control pill because I get migraines with aura and that places me at a higher risk for stroke. I had been on the pill since age 16 and this can stabilize/mask hormonal problems, so I hadn’t notice this cycle quite so much prior to 2007.
I began to track my menstrual cycle in my journal as well (years later I would have an ultrasound and be diagnosed with Adenomyosis). I was seeing a sudden intensity of symptoms 1 week prior to menstruation and then notice that somewhere around day 3-4 of menstruating, I would feel a huge relief and feel “like my old self again”. That raw feeling was gone,my anxiety was much lower. I was happy, full of energy and had much hope for my future.
Once I knew this cycle, and could track when it was coming, I was in a much better position to make some lifestyle changes during this time and to be more compassionate with myself.
Within the first few hours of “that feeling” coming back, I would label it as hormones, and use my strategies for managing my thoughts/emotions/behaviours. “That feeling” was a sudden intensity of sadness/worry. All humans feel sad and worry, but with anxiety/depression/pmdd, it’s much more intense. This is more than PMS.
We know that women who have PMDD have their serotonin levels impacted by hormones and this impacts mood and physical symptoms. I no longer had to question why I was on this rollercoaster or shame myself for it.
PMDD is serious. Up to 50% of women who have PMDD have had thoughts of suicide and up to 25% have had a previous suicide attempt. The women I have worked with have so much shame for what they feel/think/do (or not do) during this time. And it happens on a monthly basis FOR YEARS. I now ask each female client if she notices a connection between her hormones and her mood/anxiety. If so, I give her the symptom tracking sheet so we can start to watch for the pattern. You can download a copy of the tracking sheet in my Free Online Digital Health Hub.
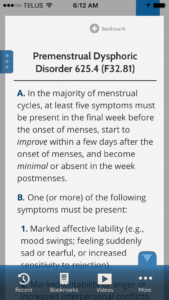
To meet criteria for PMDD in the DSM-V (which is a book used in North America to classify psychiatric symptoms into different psychiatric/mental illnesses), a woman must experience:
During most menstrual cycles during the past year, at least five of the following 11 symptoms (including at least 1of the first 4 listed):
• Markedly depressed mood,feelings of hopelessness, or self-deprecating thoughts
• Marked anxiety,tension, feelings of being “keyed up” or “on edge”
• Marked affective lability (eg, feeling suddenly sad or tearful or experiencing increased sensitivity to rejection)
• Persistent and marked anger or irritability or increased interpersonal conflicts
• Decreased interest in usual activities (eg, work, school, friends, and hobbies)
• Subjective sense of difficulty in concentrating
• Lethargy, easy fatiguability, or marked lack of energy
• Marked change in appetite, overeating, or specific food cravings
• Hypersomnia or insomnia
• A subjective sense of being overwhelmed or out of control
• Other physical symptoms, such as breast tenderness or swelling, headaches, joint or muscle pain, a sensation of bloating, or weight gain
The symptoms must have been present for most of the time during the last week of the luteal phase (the phase just before menstruation), must have begun to remit within a few days oft he onset of menstrual flow, and must be absent in the week after menses.
It also has to have impacted your daily functioning in either social, school, work or sexual functioning.This also has to be related directly to menstruation and cannot be an exacerbation of another mental illness such as depression and anxiety. And all of this has to have happened for at least two full cycles of hormones.
Now having said this, if you already have a mood disorder or an anxiety disorder that is well managed, but you notice that your symptoms are intensified during times of hormonal change, I think it’s important to share this with your doctor or your therapist. The DSM-V has good things about it and not so good things about it (that’s a whole other book) so just because you might not meet criteria because of a pre-existing mental illness, doesn’t mean your hormones aren’t playing a role in your symptoms.
You may choose to explore medication options (there are options for medication as it relates to changing hormones/serotonin) please discuss this with your doctor/psychiatrist. Or you may choose therapy. Regardless, it’s important to share this information with whomever is a part of your health care team.
A great website that I recommend to all my clients is https://giaallemandfoundation.org/ Many doctors don’t screen for PMDD, not because they aren’t aware of it or don’t care, but because they are usually helping people with other medical issues at the same time and if they aren’t seeing you on a regular basis, they may not see this cycle happening for you.
This website has information that you can share with your doctor. I’ve worked closely with over 70 doctors and they have all been supportive of PMDD once it’s been tracked as it enables them to provide better patient care.
This article is for educational purposes only. Please consult with your doctor or psychiatrist to discuss diagnosis and treatment.


Europe, and in Ancient Russia